#22: Congress’s Digital Health Directive
Representatives Kelly + Balderson hope to shape the future of digital health.
A decade ago, the term “digital health” was synonymous with telemedicine. Today, however, it has taken on a whole new meaning. From mental health apps to sleep-tracking wearables to AI-enabled chronic disease care platforms, digital health has evolved to transform healthcare delivery and patient outcomes.
While startups continue to develop more solutions, we are approaching a crossroads. Future innovation is contingent on regulatory and funding environments, and whether or not insurers will pay for digital health solutions. Congress, of all groups, hopes to influence the next decade of digital health innovation through a new Digital Health Caucus.
Representatives Robin Kelly (D-IL) and Troy Balderson (R-OH) introduced the caucus intending to advance digital health tools while ensuring all Americans will benefit.
The five focus areas include:
Informing Policymakers
Ensuring Accessibility
Promoting Collaboration
Addressing Regulatory Challenges
Advancing Research & Development
In theory, these all sound great. However, there already exists designated congressional caucuses for mental health, black maternal health, rural health, public health, and healthcare innovation—all aspects of healthcare still significantly overlooked, underfunded, and miles away from improvement.
So how can the new caucus actually improve digital healthcare?
Make Way
> Reimbursement
Digital therapeutics, such as remote patient monitoring (RPM) and remote therapeutic monitoring (RTM) technologies, are still nascent in their integration into healthcare. The Center for Medicare and Medicaid only passed CPT codes for RTM in 2022.
The path for broader coverage (new/updated reimbursement codes) of digital therapeutics is evidence-based. As payers, patients, and providers grasp the capabilities of RPM and RTM, the digital health caucus should pilot digital health tools within Medicare and Medicaid to assess cost-effectiveness and health outcomes. Virtual musculoskeletal (MSK) health companies, in particular, are already capitalizing on the RTM codes to improve patient engagement while increasing revenue for providers.
For the time being, however, payers are less likely to cover digital health solutions. A new Peterson Health Technology Institute (PHTI) analysis reports virtual diabetes management solutions “increase healthcare spending” and “do not deliver meaningful clinical benefits.”
A PHTI analysis of MSK virtual solutions is coming soon.
> FDA-Designations
There exists a bold line, drawn by the FDA, between fitness & wellness trackers and medical-grade devices. But as consumer wearables gain Class II and Class III clearance, that line is getting blurred. Wearables are an asset to public health, whether designated as medical-grade devices or not. Consumer devices assist in the management of chronic conditions and in some cases can detect serious health issues (think Apple Watch detecting Afib).
The FDA themselves have created a new advisory committee for digital health and AI set to become operational this year. Close collaboration between the committee and Congress’s digital health caucus will likely see the expansion of the Digital Health Software Pre-certification program. As part of the program, the FDA will forge a streamlined path for future clearance and approval of impactful health technologies by being involved in the validation and design of products. Such technologies could include other wearables like continuous glucose monitors for non-diabetics.
Data Makes the World Go ‘Round
> Interoperability + Data Privacy
Consumer health data hasn’t yet met clinical standards. Nonetheless, patients are increasingly choosing doctors who use wearable data. It’s only a matter of time before consumer wearable data will be integrated into EMR and EHR systems (perhaps with an AI-screening layer).
The digital caucus will play a critical role in advocating for standardized data protocols and updating HIPAA guidelines to protect patient data shared between wearable companies and electronic medical record systems.
If data from digital health tools become aggregated, there is huge potential for gaining insights into public health trends and treatment efficacy, which will even inform future health policy.
Money Talks
> Funding/Grants
In 2023, digital health venture funding was just $10.7b, the lowest allocation of capital since 2019.
The caucus can potentially create federal grant programs for digital health startups, especially those increasing access to healthcare for underserved populations. Similarly, an accelerator program at the federal level could promote more digital health innovation.
Look for the committee to fund startups in spaces like obesity care, food-as-medicine, and AI.
> Digital Health Infrastructure
As it stands, digital health has some serious barriers to entry. Improving access to internet and technology literacy should be top priorities for the digital health caucus, given that internet is considered a superior determinant of health, with 19 million people in the US lacking reliable broadband service. Subsidizing internet service for rural areas will enable telehealth and other digital health services for underserved populations.
Other investments should go into storing data locally, using less bandwidth, and creating a closed-loop digital health system within homes.
“Remote connectivity exists in almost every other discipline or profession, especially in the tech world. And so we just need to learn from them and learn how to do it.”
~ Dr. Ami Bhatt, Chief Innovation Officer of the American College of Cardiology
Digital Health is…Health
Our digital health footprints—patterns of technology use—are becoming massive. Patients are interfacing less with providers and more with their devices for healthcare needs. For the disruptive healthcare companies of the future, digital health is not just an add-on. It’s a necessity.
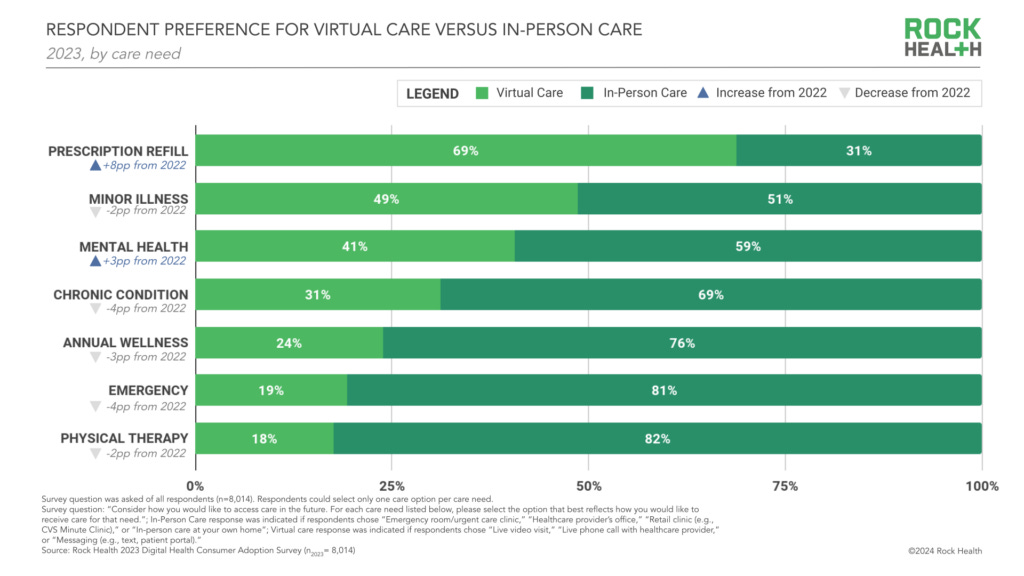
And although consumer preferences aren’t completely virtual, the future of healthcare will be a mix of in-person and digital interactions.
“The important takeaway is that, for most consumers, virtual care is now a fixed expectation on that spectrum. But even virtual adopters sometimes prefer in-person care for certain health needs, further building the case for a spectrum of omnichannel approaches.”
The government—like healthcare in general—is slow to adopt change. But the new digital health congressional caucus will hopefully catalyze another decade of healthcare innovation.
What I’m Reading:
END THE PHONE-BASED CHILDHOOD NOW, The Atlantic
Medicare Opens Door for Covering Obesity Drugs, WSJ
Growing with creativity and authenticity: Lessons from Digital Health CEO Summit 2024, Rock Health
During the pandemic, were great vaccines bad business? A company-by-company review, Stat
Latest Podcast Episode:
Listen Here.